Dunedin Hospital has "never really been close" to meeting the Ministry of Health target that orthopaedic patients receive planned care within four months, and the situation is getting worse, the service’s clinical director says.
At present, 947 people have been told that they are to have a procedure but more than 750 of those have waited more than four months for a date, Michael Chin told the Southern District Health Board’s hospital advisory committee yesterday.
That was due to a "perfect storm" of longstanding wait lists, Covid-19 lockdown postponements, staff shortages and related bed closures, Mr Chin said.
That had been exacerbated by no spinal surgeon working in Southland for at least 12 months. All regional referrals were now sent to Dunedin, where the spinal team’s patient list had doubled.
"It has been worse in recent times with cancellations on the day, usually due to bed block, and particularly due to a lack of high dependency and intensive care beds, but more recently on the wards," Mr Chin said.
"We are being overwhelmed with acute cases but also still trying to maintain electives."
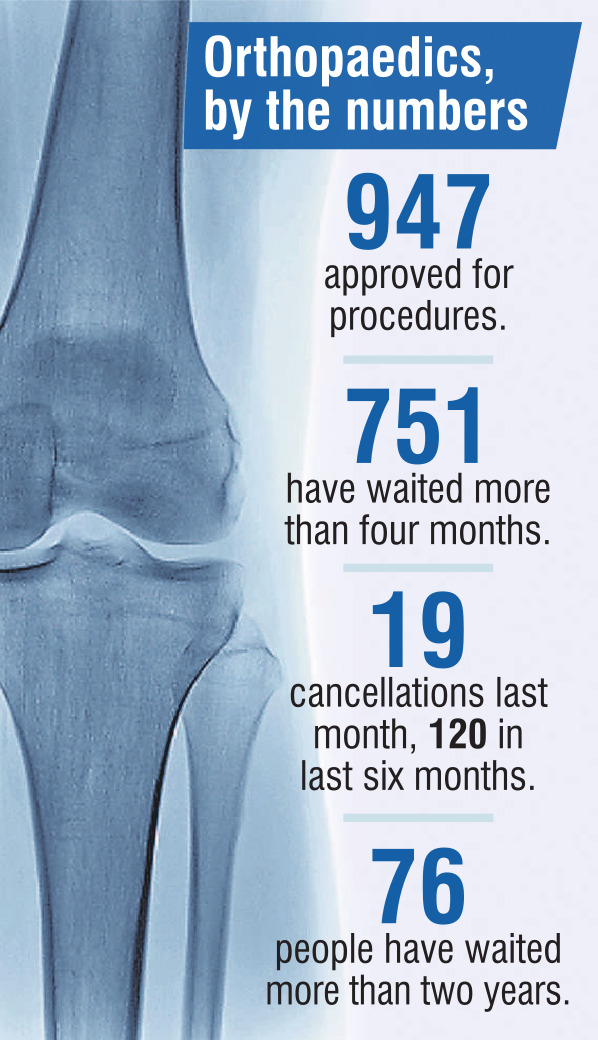
An average of 21 operations a month have been cancelled during the past six months, but during that time the service had been deliberately under booking procedures to try and avoid postponements, Mr Chin said.
This year the service was only likely to deliver 80% of the operations it did seven years ago, let alone its actual projected numbers, he said.
"That is with an increase in outsourcing which has occurred over the past two years."
Demand for orthopaedic surgery meant the average 220 referrals from GPs a month had to be triaged, and almost half were sent back to their doctor, Mr Chin said.
That meant when patients finally did get to see a specialist a high proportion required surgery because their condition had deteriorated in the meantime.
"We are reasonably well staffed with senior medical officers, but our problem is that we have a lack of operating time and the things that factor in to that are particularly a lack of staff, and the lack of anaesthetic technicians in particular has been an ongoing problem," Mr Chin said.
"Nursing staff has come to a head and we have had issues in the operating suite and more recently it has become apparent in the wards."
Extra surgical lists had been added later on weekdays and in the weekends, but the service was still under severe strain, Mr Chin said.
"The delay in getting the ICU redevelopment online has meant that lots of more complicated patients, which unfortunately are making up an increasing part of what we do, are winding up being delayed getting into surgery because we just don’t have the space, and often we don’t know until quite short notice when that is happening."
Initiatives to manage the issue included sending 70 patients a year to South Canterbury, utilising capacity at Mercy Hospital, and better managing patients in the community until a slot became available for them to be treated.
Recruitment campaigns were continuing, and the service also wanted to ringfence some beds for high turnover elective procedures, Mr Chin said.
Comments
I had cause to apply for ACC funding dur to a little accident recently. ACC sent me a questionnaire via text a couple of days after "How did we do" I said all was good great response time etc they then asked me "anything else to say" I said ACC should help to fund the hospitals. Not rocket science when that is where they are directing their clients. Where do all our Medical Uni grads go and why?












