It was during the last fortnight of January that James Ussher dropped by Miguel Quinones-Mateu’s seventh floor corner office for a chat about growing cases of a then-unnamed coronavirus.
"Hey Miguel, have you seen what’s going on in China?" Prof Quinones-Mateu recalls his colleague asking.

"Well, you have experience developing molecular diagnostic assays. Do you think we should try to put something together, in case that virus makes it to New Zealand?" Prof Ussher, an infection and immunity specialist, suggested.

So that is what they did; obtaining synthetic genetic fragments of the virus in order to verify a system that could be used by medical laboratories to test for Covid-19 infection, should the virus arrive.
"There was a lot of under-the-hood stuff that we had to get sorted out to make that work,"Assoc Prof Ussher says of the collaboration between the university and the Southern Community Laboratory, in Dunedin Hospital, for which he is also a pathologist.
"We finally got that running on Friday, March 13; the same day we got the first positive case [of Covid-19] in Southern [District Health Board area]."
Ten days later, as the country went into lockdown, the handful of PC3 labs were closed down, except for the one in Dunedin.
"I wanted to keep it open to be able to work with the virus," Prof Quinones-Mateu says.
"Having access to this PC3 has made it possible for us to do everything we have been doing for the past four months."
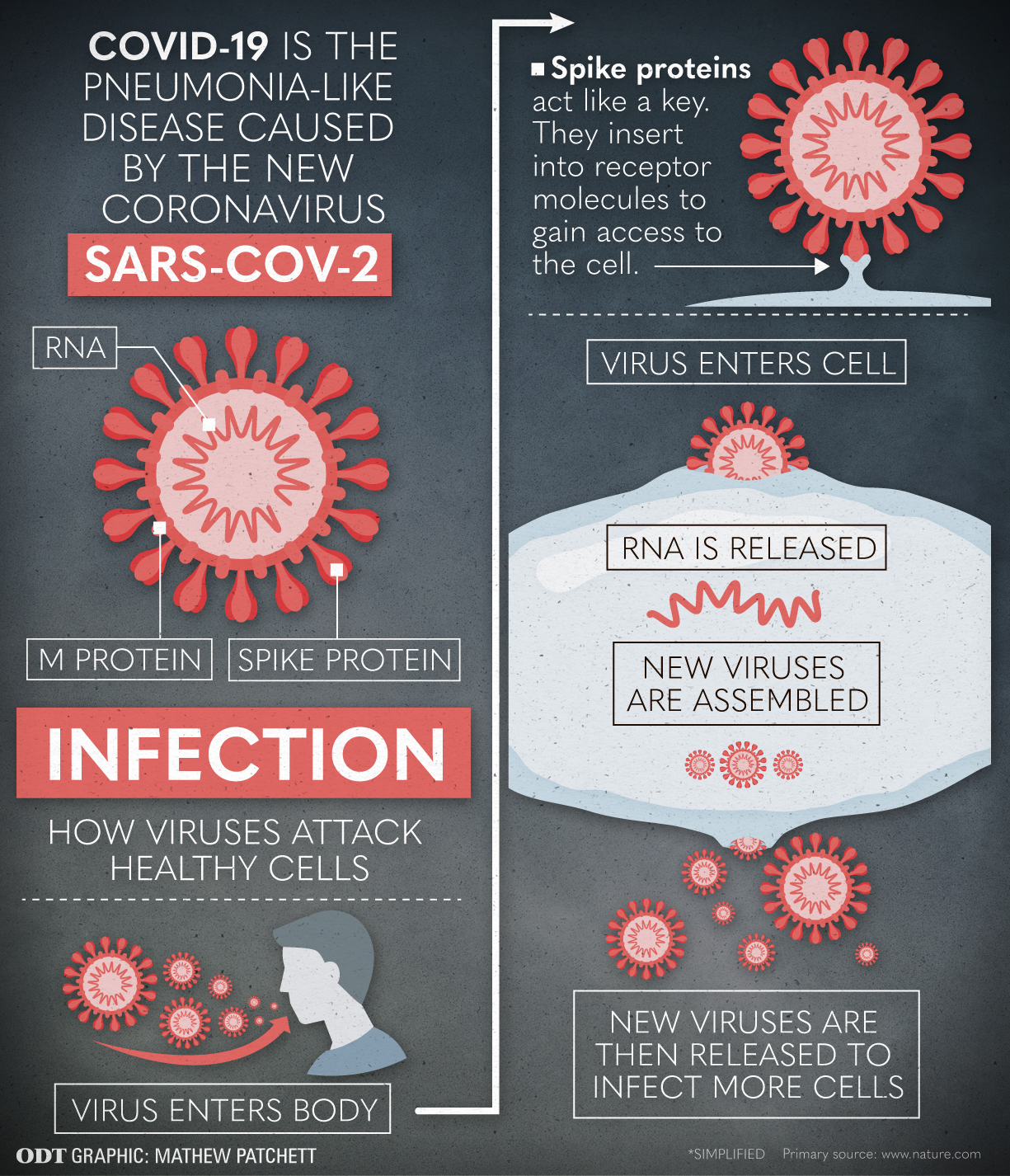
Positive cases and access to a high-containment lab meant his team was able to grow the SARS-CoV-2 virus and isolate its RNA, its genetic material; the first New Zealand lab to do so.

"I have a list of more than 20 groups contacting me to work with, you name it, any compounds they want to test against the virus to see if it has antiviral properties; vaccine development; how to kill the virus, for example, detergents or UV light so that PPE can be reused; clinical studies ..."
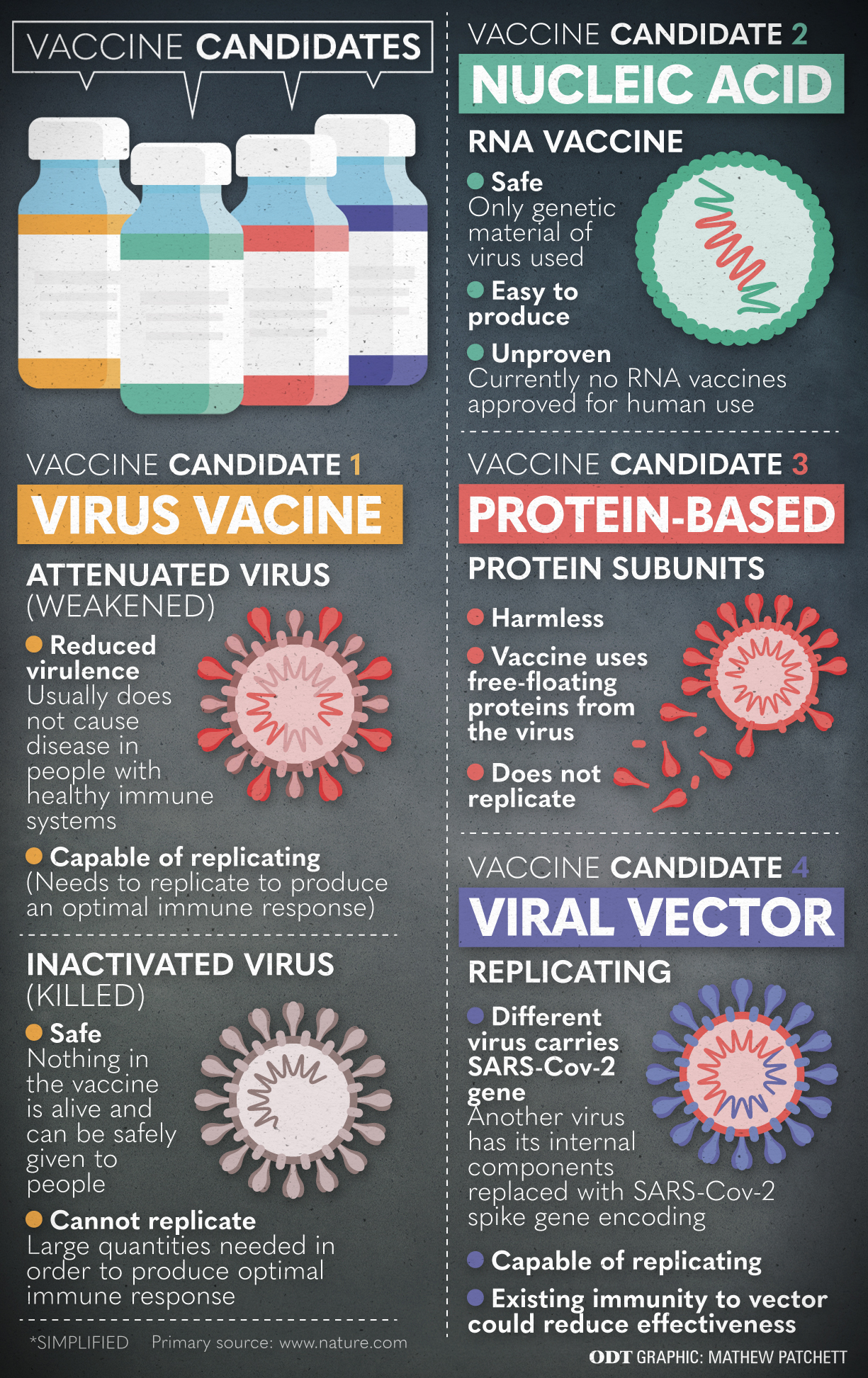
Early on, professors Quinones-Mateu and Ussher made the decision to start researching a SARS-CoV-2 vaccine.
"This is what we do. We have the tools, we have the PC3 laboratory, we have the expertise, we have the people. Why can’t we join the fight? Why do we have to sit down and wait for Europe, the US or Australia to do all the work?" Prof Quinones-Mateu says, explaining their reasoning.
Prof Ussher was vocal and persistent in his call for the Government to fund national efforts to produce an effective SARS-CoV-2 vaccine.
"We might have eliminated the virus here ... but it is going to continue to circulate globally," Prof Ussher says.
"As soon as we relax our border restrictions ... it will be very difficult to stop it from coming back in. So we need a vaccine to allow us to have some sort of return to normality."

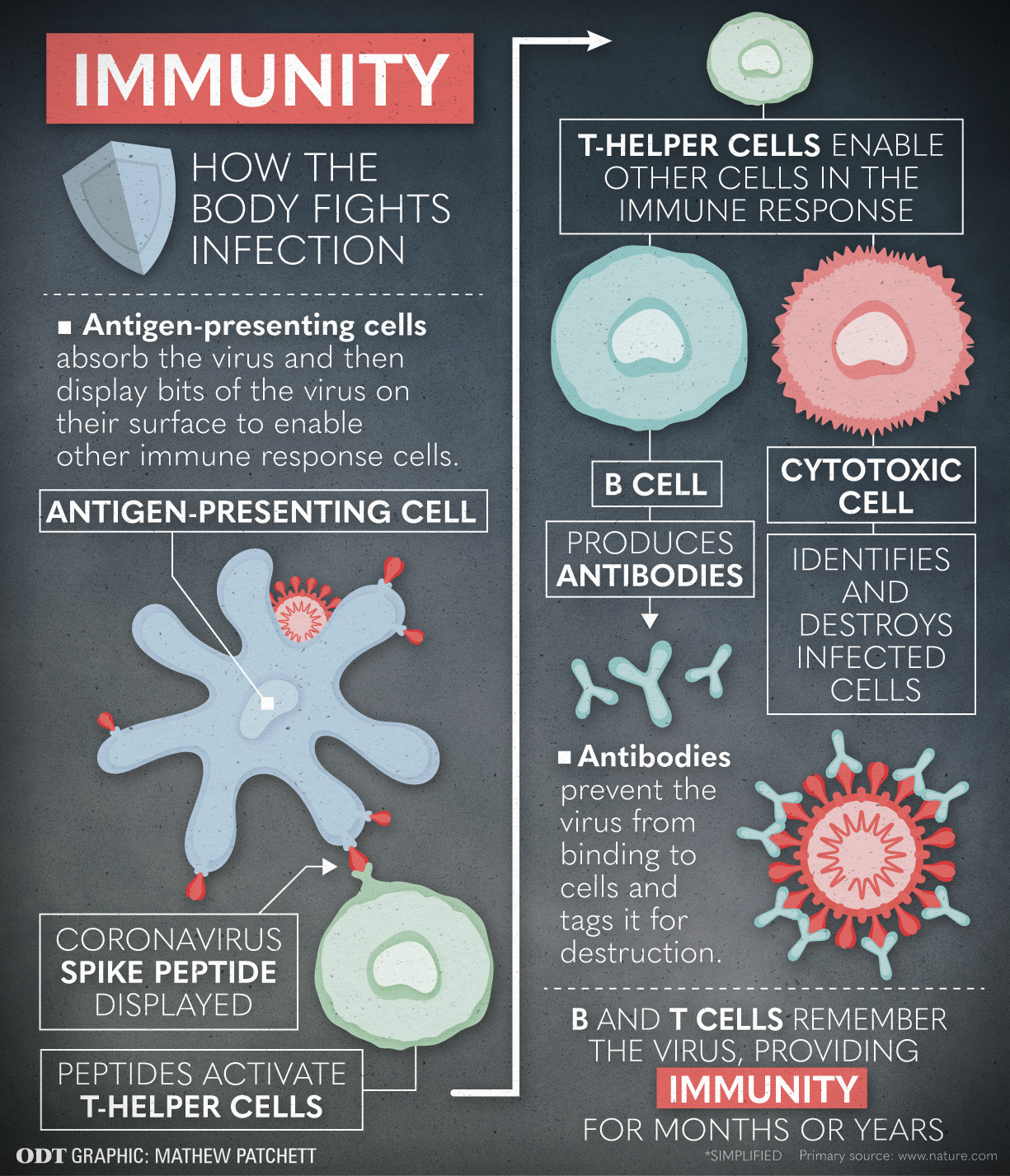
"We don’t know what protective immunity to SARS Coronavirus looks like. There are over 130 vaccine candidates globally in development now, but how many of those will be successful is unknown. So, we need to contribute to that global effort."
New Zealand also needs to be involved in vaccine research and manufacture because it will be years before we get access to a vaccine if we do not have some skin in the game.
"There is a significant risk of countries being possessive of what they manufacture.
"The Serum Institute of India, who are manufacturing the Oxford vaccine [in anticipation of trials proving successful], have said they can’t envisage shipping vaccine overseas until they have vaccinated the Indian population."
Manufacturing in New Zealand would also help ensure Pacific Island states get a vaccine.
The Government listened. A fortnight ago, Deputy Prime Minister Winston Peters announced a National Vaccine Strategy that came with a $37 million budget. Almost half will be for New Zealand research and manufacture, a further $15 million is for international research collaboration and $7 million will fund vaccine distribution in developing countries.
The money is "fantastic" and "the best way for New Zealand to contribute to the global effort", Prof Ussher says.
"The Government’s commitment to local vaccine development enables us to push on with our efforts at the University of Otago."
His "best case scenario" prediction is that it will take 12 to 18 months for a successful vaccine candidate somewhere to be identified and go through clinical trials. It will then need to be manufactured and distributed.
Prof Sunny Collings, who is head of New Zealand’s Health Research Council, also applauds the Government for "showing international leadership" by funding vaccine research.
"This has shown New Zealanders in a real way the value of decades of investment in our health research system," Prof Collings says.
"Perhaps we have never seen such an immediate and practical impact of health research on people’s daily lives."
Otago researchers on campuses throughout New Zealand are taking a leading role. Some are now household names, others are not so well known, yet. Bruce Munro talks to Dr Ayesha Verrall, Prof Michael Baker, Assoc Prof Jo-Ann Stanton and Dr Jemma Geoghegan about what they are doing, why and what needs to happen next.Dr Ayesha Verrall told New Zealand its contact tracing system was not up to scratch. Now she says we need to ask whether we’re really ready for a pandemic repeat.
In the middle of Level 4 lockdown, Ashley Bloomfield, director general of health, asked the infectious diseases physician and researcher from the University of Otago’s Wellington campus, to tell him and the nation whether our contact tracing capacity could meet the challenge of going to Level 3 and lower.
Her assessment, diagnosed in one day and written up in two, using a technique learned working for the World Health Organisation, was summed up in a tweet she posted.

The Government listened, releasing a further $55million and 300 staff.
Since then, she has been busy sharing what she has learned. For instance, advising UK health officials on how to implement large scale contact tracing New Zealand-style.
However, Dr Verrall says we still have a lot more to understand and important lessons to learn.
One interesting question she wants to pursue is, why, for most people, is there a low virus transmission rate, when, at the same time, we have seen cases of big clusters?
"So, what are the factors that led to clusters of infections?"
One possibility is that some people have cross-protection from other coronaviruses that circulate as the common cold.
"But, that’s a maybe," she says.
Dr Verrall says it is important to look at these things because we probably are not as ready for another pandemic as we should be.
"When the dust settles we do need to think about what the right institutional arrangements are for responding to infectious diseases in the future."
Recalling a week during February when the pandemic appeared to be an all-consuming tsunami, Prof Michael Baker chokes up.

Advising the Government and public on the likely spread and impact of the pandemic, urging officials to take the steps needed to eliminate it, answering media calls at all hours, sleeping little more than five hours a night for weeks on end — it has taken its toll.
"It has been the most intense experience of my life," the head of public health at the university’s Wellington campus admits.
The worst days were before the Level 4 lockdown, when Prof Baker was being outspoken in his calls for drastic action but was not sure he was being heard.
"I felt New Zealand needed to move much faster in response to this pandemic threat at every point," Prof Baker says.
"I felt quite often out on a limb giving a view that was not necessarily supported by everyone and where the evidence was not yet complete."
Dr Baker urged the Government to take a containment approach and aim for elimination of the virus within our borders.
Embracing an elimination strategy in a timely way has paid big dividends, he says.
"With an elimination approach you don’t ... try to flatten the curve, instead you throw everything at it at the start.
"If we had delayed much longer it would have been very hard to extinguish the virus."
Although life was still frantic, Dr Baker found he slept better once Level 4 was announced.
"I loved going to sleep knowing the virus was fizzing out around the country."

Imagine those staff working long hours to process and test swab samples sent from around the country so that patients and their carers can be told whether they are positive for Covid-19.
Now imagine a nurse or customs officer in a country clinic or an airport office with a single portable box. They feed a swab sample in to it. Within the hour, a read out tells them whether or not the person is infected or clear.
The first scenario is now. The second is what Assoc Prof Jo-Ann Stanton is working hard to make a reality.
For the past two-and-a-half years, the anatomy department researcher has been using a government Endeavour grant to develop a device that would enable people unfamiliar with complex molecular diagnostic tests to do just that.
When the pandemic came along, Prof Stanton focused her efforts on developing a device that would specifically test for Covid-19.
The work is being done in collaboration with researchers and clinicians throughout the country.
In six months, she hopes to have a working model close to completion. It will not yet be a single box, but will have all the component parts to allow a trained user to get a reliable result "in the field".
The ability to do tests in more locations and get results quickly will be important when border controls are lifted.
"Even though New Zealand is coming out of extreme pandemic mode, the rest of the world isn’t," Prof Stanton says.
"Whether it is for work or tourism, people are going to come and go.
"So, the testing programme has to continue."

Dr Geoghegan trained as an evolutionary virologist at the University of Otago and was just returning after a decade of international research when the pandemic struck.
She has hit the ground running, forming and leading a nationwide research group that has been awarded funding to sequence the genomes of the SARS-CoV-2 viruses identified in each of the country’s 1154 confirmed cases.
Interesting in itself, the research will also allow the scientists to map how the virus spread both through time and in space.
"From that we can understand how effective the different intervention levels were in stopping the virus spreading ... and we can understand whether there is any undetected community transmission."












