Wanaka’s demand for 24-hour after hours primary care is taking place in the context of a nationwide Rural Unplanned and Urgent Care (RUUC) review.
The review has been planned for some time. Last year, there was talk of it being completed by June 2024 but that did not happen.
Health New Zealand’s website makes it clear there is still more work to be done.
HNZ expects to be identifying proposed models and future options from October this year, and have its final decision document ready for consultation by February next year.
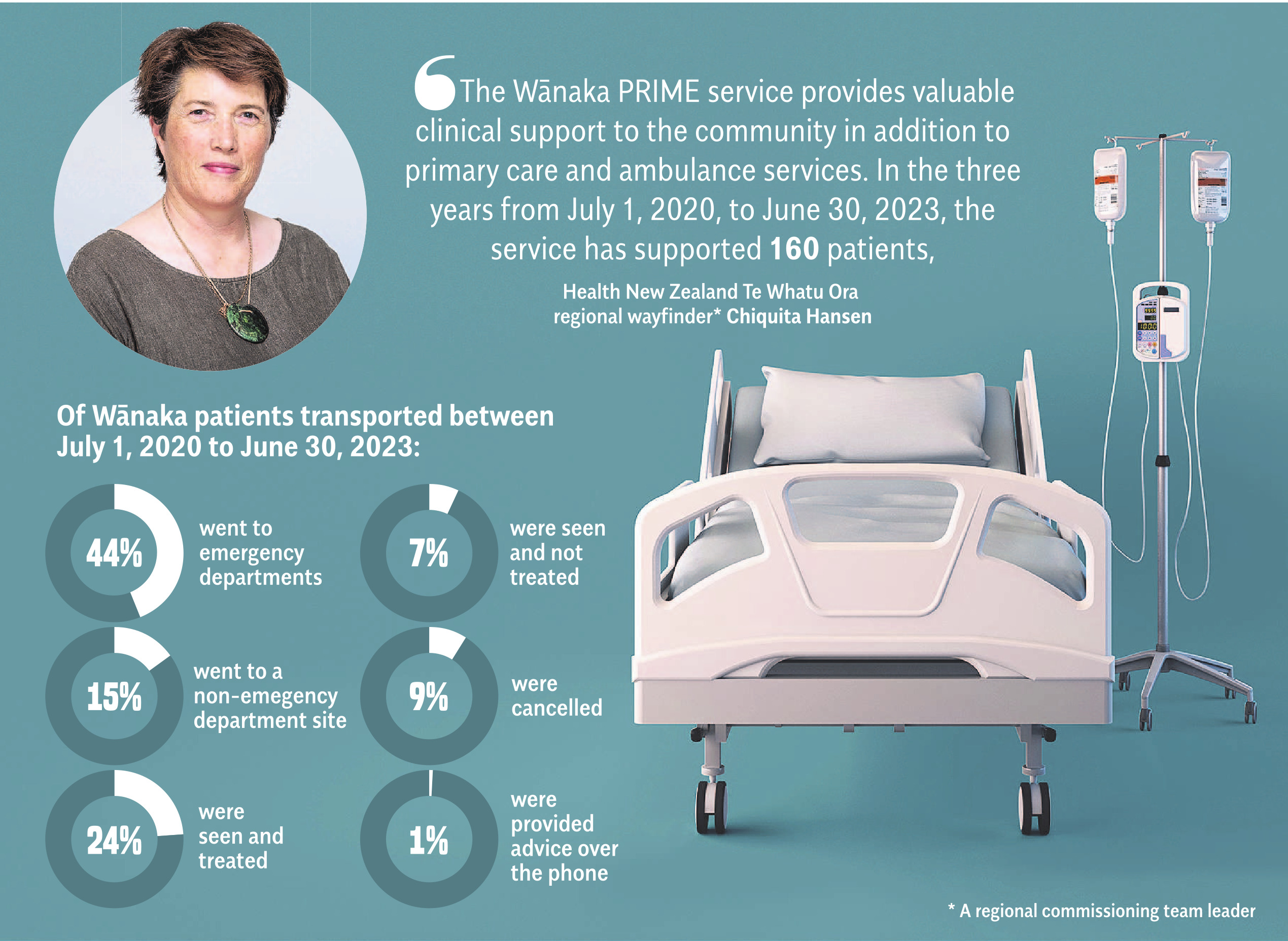
The RUUC review includes the Primary Response in Medical Emergencies (PRIME) service, which was established over 20 years ago and comprises doctors, nurse practitioners and registered nurses, helping provide a level of care in rural and remote areas to support emergency ambulance services.
Essentially, ambulance services are supported by rural health practitioners if response times could be significant, or when higher level medical skills are needed.
PRIME services and primary care after hours services are administered separately.
The structure and operating hours of the services vary, depending on local resources.
HNZ regional wayfinder Chiquita Hansen said Wānaka’s after hours care is covered by a primary health organisation agreement.
In Wānaka, this funds GP cover between 8am and 11pm.
HNZ also provides urgent care services through contracts with healthcare providers. They are:
- A new nurse-led after hours primary care service from 11pm-8am, seven days a week, scheduled to begin next month and end in August 2025.
- A national ambulance contract with Hato Hone St John.
- Rural hospital specific acute services at Dunstan Hospital, Clyde (76.4km east from Wānaka) and Lakes District Hospital in Frankton, Queenstown (62.7km south of Wānaka).
- Telehealth national contracts (Ka Ora and Whakarongarau).
- A national PRIME service, jointly funded by Health NZ and ACC and administered by St John, which is included in the RUUC review.
The Wānaka Sun requested, but was not given, the HNZ budgets for Wānaka afterhours and PRIME services.
Wānaka’s PRIME service has 18 doctors and 26 nurses across the district.
St John Central Otago area manager David Baillie said, in response to questions from the Wānaka Sun, that the jointly-funded PRIME service was "well covered in the Wānaka district, with the contract co-shared by two medical practices that provide cover... seven days a week."
Mr Baillie said St John was an integral part of Wānaka’s health care system, and collaborated with HNZ to meet health needs.
"Based on the emergency ambulance workload in Wānaka, our resourcing model is appropriate for the area and is consistent with the resourcing in similarly size towns across the motu," Mr Baillie said.
Wānaka has two ambulances most of the time, with a third ambulance added to help with the winter population increase between 10am and 8pm.
"Over the past year, the team in Wānaka has responded to on-average, 29 calls each week to the town.
"Our data indicates that most patients who required transportation — over half — are taken to a local treatment centre, meaning the local ambulance stays in the community for most of the time.
"When the emergency ambulance does need to transport a patient outside of Wānaka, our first response crew, crewed by dedicated volunteers, steps up to respond," he said.
St John had the support of Fire and Emergency NZ, air ambulance helicopters and PRIME doctors. When comparing emergency ambulance resources to other regions.
"Wānaka is well resourced for the funding Hato Hone St John receives," he said.












