
I have to say that because every March some of my behaviour can be questionable.
Call it March madness, but after 27 years I am still acutely aware this is the month my husband was buried, a few days before his 49th birthday.
It can make me a little distracted. He would probably call it discombobulated, one of his favourite words.
If you saw me wandering around the city with some freshly picked Carmine beans (the ones my Swiss ancestors brought out here in the 1800s) dangling from the tassels on my scarf recently, I forgive you for rushing to judgement about my sanity. Discombobulation in action.
But while I am asking you to excuse such odd behaviour, March madness makes me more than usually intolerant of political shenanigans, particularly when it comes to anything to do with bowel cancer, the disease which killed my husband.
The stage management around the announcement of the change to the starting age for bowel screening programme from 60 to 58 was questionable.
In December, the current government halted the previous government’s move to improve equity in the programme. This would lower the entry age to 50 for Māori and Pasifika (available in three districts to date).
These groups have a high proportion of cancers occurring before 60, their cancers are often late stage when diagnosed and they have a high death rate. They get less benefit than the rest of the population from a programme which starts at 60.
It made sense, since there was not colonoscopy capacity to extend screening to all at 50, to offer it to Māori and Pasifika first.
The coalition government did not see it that way but had to be seen to be doing something towards fulfilling the promise to lower the age to 50 for all, made under pressure on the election campaign by now Prime Minister Christopher Luxon.
In a series of interviews after he made the announcement about the move to 58 this month, Health Minister Simeon Brown referred to Ministry of Health advice he had received.
But instead of issuing the relevant documents at the time of the announcement, he did so eight days later, last Friday.
Anyone listening to his interviews before their release could have been forgiven for thinking he was suggesting he had followed ministry advice.
What a surprise: the documents showed Mr Brown and his Cabinet colleagues chose the cheapest option and rejected the recommended ministry change which would have seen the age lowered to 58 for most of the population and to 56 for Māori and Pasifika.
Over 25 years, it was estimated that move would have prevented an additional 918 cancers (compared with 771 for the move to 58 for all) and avoided an extra 678 deaths (566).
The ministry’s recommended option would not have benefited Māori and Pasifika as much as Labour’s scheme, but it would have saved 111 more of their lives than the universal 58 start.
We do not know yet how the required colonoscopy capacity is to be achieved. We do know the system overall is struggling already.
As of August 2024, only 41% and 54% of non-urgent and surveillance colonoscopies were meeting the target waiting times.
There are plans to lessen the number of colonoscopies performed outside the programme. Presumably, the rationale is that too many colonoscopies for symptomatic patients do not show up bowel cancer.
This will be done by introducing the use of the faecal immunochemical test (FIT) to triage symptomatic patients, the same sort of test which is used in the screening programme, although we do not know such details as what level of blood in the faeces will support a colonoscopy referral.
I wonder if there will be fears among referring clinicians this could make it harder to get colonoscopies for their symptomatic patients (whose cancers might not be bleeding at the time of the test).
Readers will be well aware of the concerns Southern clinicians have had about access to colonoscopy for symptomatic patients over many years.
It is also not clear how well our struggling system is placed to cope with any extra surgery and other treatments associated with finding extra cancers through the programme, which will be funded from Health New Zealand’s baseline.
While I would love screening to begin at 50 or 45, getting there will involve comprehensive planning, not evident in the current approach.
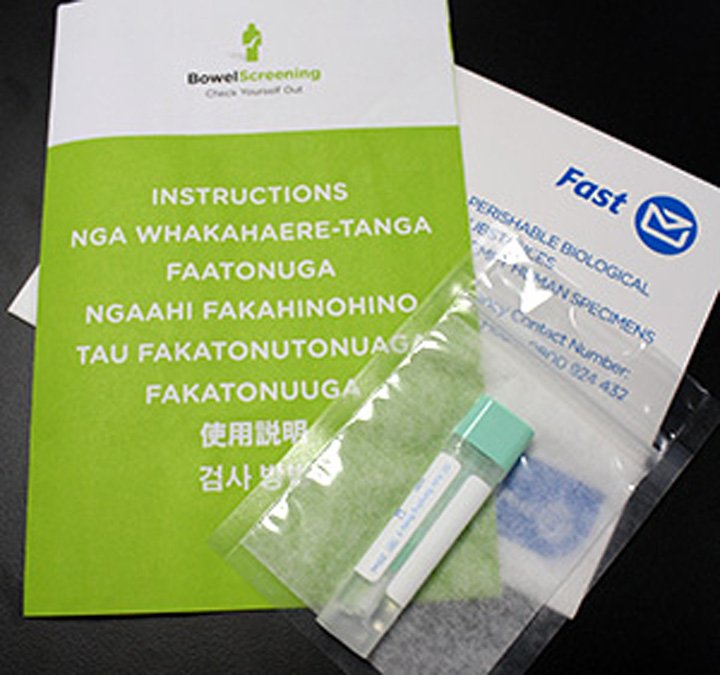
It’s not a matter of posting out a few more FIT kits. Ensuring there is equity, comprehensive information for participants, high participation, efficient laboratory services, timely access to colonoscopy for all those who qualify, capacity for timely surgery and other treatments and adequate follow-up, and top-notch independent monitoring and evaluation all come into the mix.
Mr Brown et al have shown limited understanding of much of that, and it is not OK.
• Elspeth McLean is a Dunedin writer.












