
The New Zealand Herald was sent photos from a disgruntled visitor showing a patient, this week, waiting under the leaky tent outside the hospital's emergency department. With the photos, the visitor wrote: "state of our health system".
The tent area is part of a Covid triage system in an attempt to keep the virus away from patients. It has been in place for more than two years and hospital officials stressed "patients didn't stay there for long" before they were moved into a "solid cabin" and then ED.
As of yesterday, North Shore Hospital had 108 active Covid-positive inpatients - the most for New Zealand's hospitals.
The Herald agreed not to publish the photo of the elderly patient for privacy reasons.
The photos come after a survey - conducted by the New Zealand Women in Medicine (NZWIM) Charitable Trust, including responses from more than 900 New Zealand doctors - warned a "catastrophic collapse" of the healthcare workforce loomed.
"Ward full, extreme staff shortages, ED full and seeing little babies as young as seven weeks old waiting (more than) >2 hours outside in tents for a bed in the department, or to be seen and an attempt at an exam made in the tent," one junior doctor working in paediatrics said in the survey. The hospital where this doctor worked was not specified.
In response to the photos, a spokesman for the New Zealand Nurses Organisation (NZNO) said: "An elderly woman huddled in a blanket in the freezing wet and cold outside ED starkly illustrates the very real human cost of successive governments' failure to address the health care and nurse staffing crisis."
"More nurses would mean more available ward beds and quicker triage, meaning less crowding in ED," he said.
Another union leader spoke generally on the continued strain hospitals were under with a surge of Covid and winter bugs.
Nurses Society of New Zealand director David Wills said everyone was doing their best but services were overwhelmed by Covid, influenza and RSV.
"Waitemata has 141 Covid-19 cases at present."
"Risk mitigation and preventing cross-infection is important, especially given the current surge in Covid numbers. Triaging in a tent in winter rain might not be ideal, it is arguably better than putting patients at risk," Will said.
A Te Whatu Ora (Health NZ) Waitematā spokeswoman said patients did not stay in the soft tent area for long but transitioned from "solid cabins outside" to ED via the tents.
"Auckland experienced extreme rainfall and weather conditions on Tuesday morning, including in the Waitematā area which resulted in minor pooling of water in our Covid-19 triage tents.
"We acknowledge those patients who were affected by the impacts of this weather while in our care and apologise for any distress caused," she said.
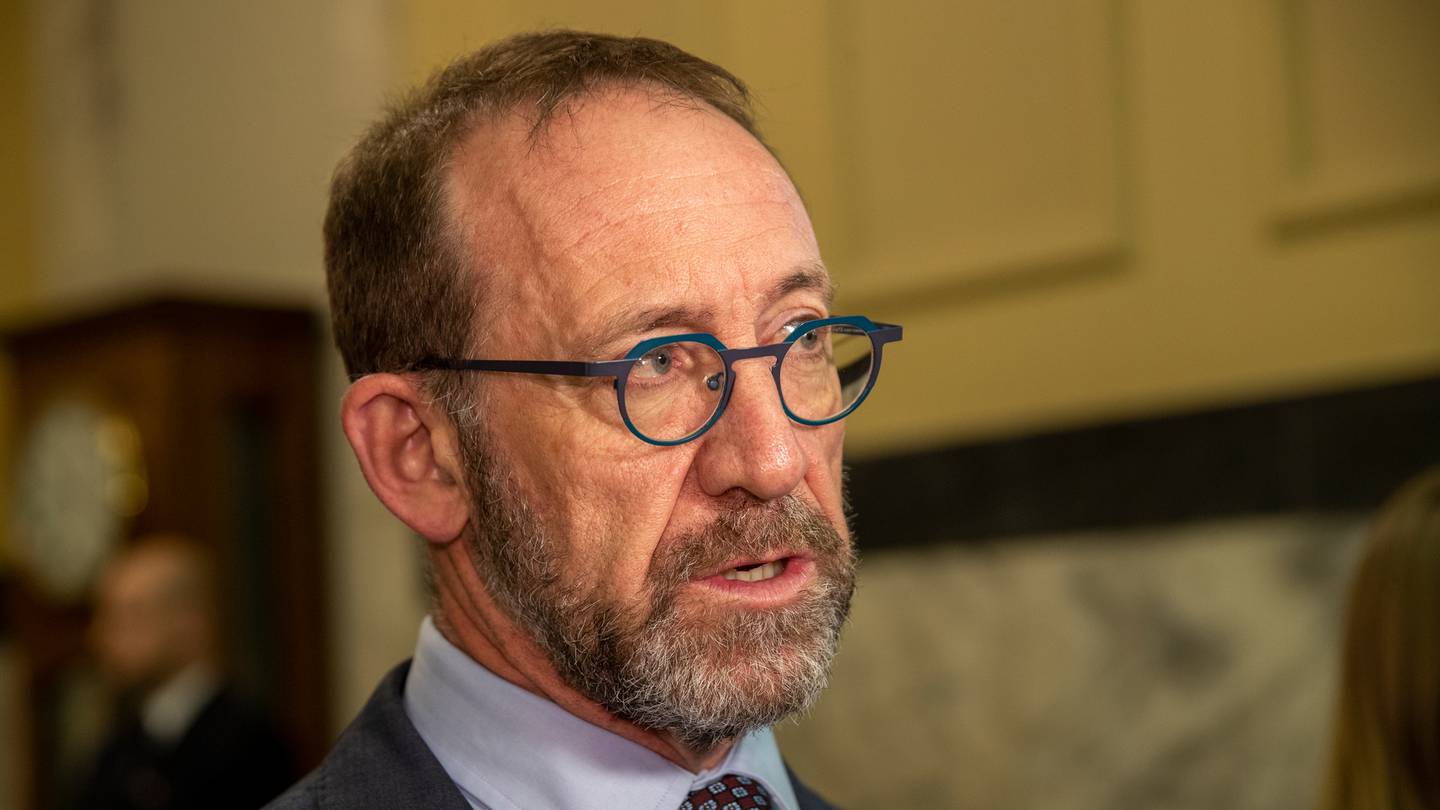
"It is putting extreme pressure on many parts of the system. I'm confident that the clinical and management leadership of our hospital system is responding appropriately and doing the best that is possible in the circumstances, and is giving the support to the frontline health workforce that I expect it to be provided," Little said.
He said recruiting staff was the Government's top health priority.
"Since coming into government in 2017 we have employed an extra 5700 doctors and nurses to work in public hospitals. Overall, the country's clinical workforce has grown by more than 11,000 over that time to almost 100,000."
"We're also training more nurses than ever, brought 5700 critical healthcare workers in through MIQ while the borders were closed, changed the immigration rules to make it easier than ever before for health workers to enter the country and have got multiple recruitment campaigns under way, here and overseas," Little said.
Last month, a "healthy" 50-year-old woman died with brain bleed after allegedly being told by staff at Middlemore Hospital's ED there would be an eight-hour wait before she was examined.
She presented with a severe headache at 1am and left due to the wait. By the time she returned it was too late.
The hospital launched an investigation into the circumstances that led to her death. Te Whatu Ora (Health NZ) interim district director for Counties Manukau, Dr Pete Watson, didn't respond to questions on when those findings were expected but did say once the review was complete he would provide a public statement.












