
"Health Care Home" sounds like something a marketing department might have dreamed up.
"A trip to the doctor sounds stressful; maybe a visit to the health care home would be more reassuring?"
However, it is a concept the American health system has been using and modifying for more than 50 years.
Initially aimed at children with special needs, it has evolved to cover all areas of practice, with the intention of addressing issues of equitable access to health services and better managing long-term chronic conditions.
The idea has gained acceptance internationally — Australia began opening HCHs in 2016, and New Zealand’s first HCHs opened in 2011.Around 130 New Zealand practices have adopted the model, serving an estimated one million patients.

Applications for general practices to become HCHs were over-subscribed: the four practices announced as HCHs a week ago will be followed by another 12 in the next year.
A further call for would-be HCHs will be made next year; ultimately health officials hope all GP practices will become HCHs.
Health officials and practitioners alike are open about HCHs being novel, and that there is some uncertainty how the HCH model will work in each individual GP practice.
The general idea however, is grounded in "patient-centric" medicine: each individual manages and organises their own healthcare, depending on their preferences.

HCHs are also intended to be accessible, which is where the SDHB — the most far-flung DHB in New Zealand — starts to get really interested.
Patients will be encouraged to use an online "patient portal" for tasks such as organising appointments, renewing prescriptions, asking questions, accessing test results and consulting their notes.
The SDHB hopes this and other tools such as telehealth — using the internet and/or mobile phones to deal with clinicians — will improve access for health services for those in remote areas.
This will be one of the major changes for GP practices shifting to become an HCH — the system emphasises accessibility and flexibility, so either more medical staff will need to be taken on, or their working hours will change.
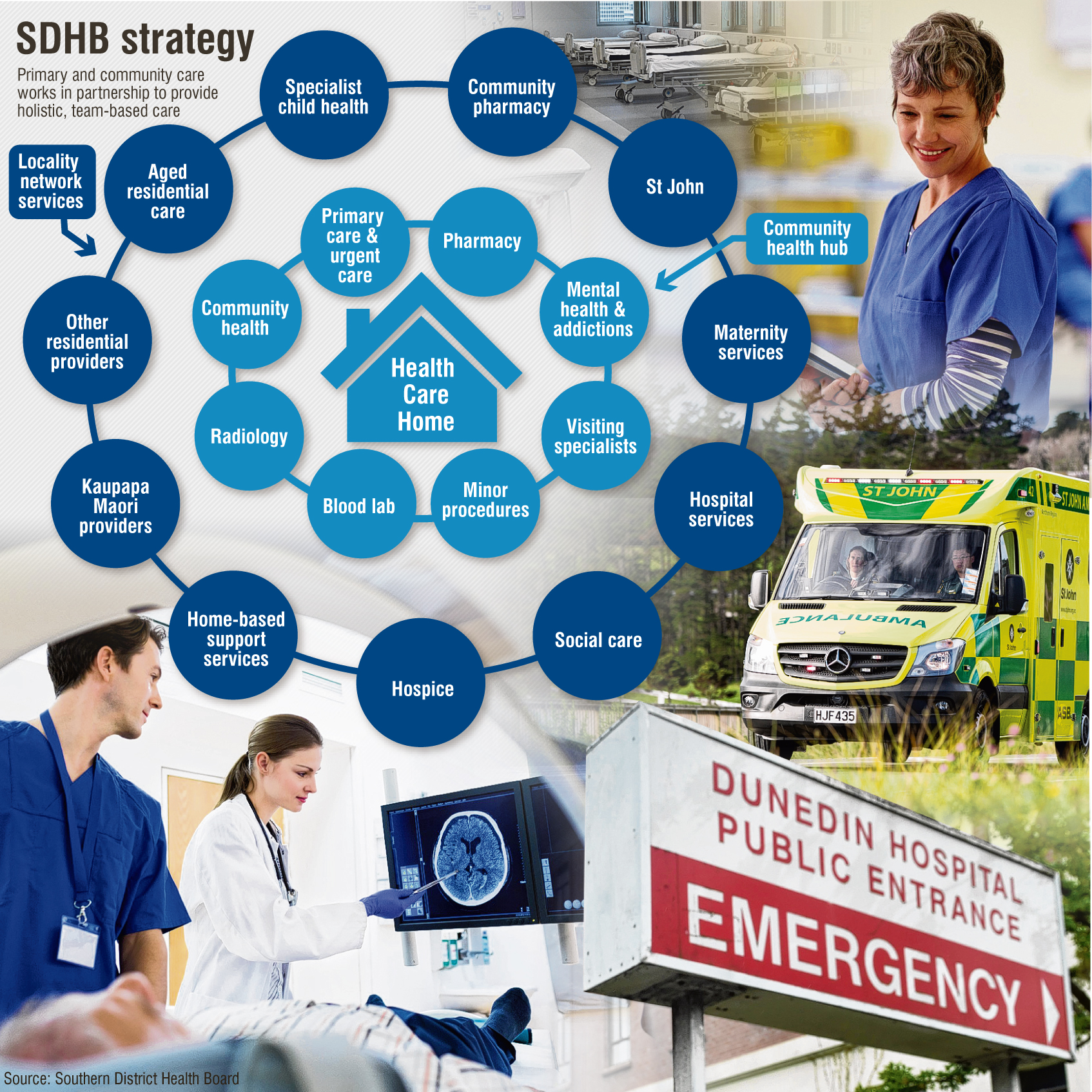
For patients, it should mean easier access to more information, more services, and greater flexibility about when they make appointments.The ultimate aim, once HCHs are in place, is to create Health Care Hubs — one-stop shops providing a range of health services.
While the basic idea seems sensible — for example, a patient with an appointment with one clinician can be booked to see others around that time, eliminating travelling and double-handing information — it also raises questions about access to patient records.
Privacy commissioner John Edwards recently called for health privacy rules to be overhauled, and the Auditor-general has reviewed patient portals specifically — saying anecdotally they seemed to be working well, but further assessment was needed.
While sold as patient-centric, it’s not like there isn’t something in this for health providers too — it is hoped Southern will follow international experience and see a drop in ED presentations, as well as people with ongoing chronic health conditions being able to stay in their own homes for longer, rather than being in hospital or residential care.
"Fundamentally, it’s good for patients," SDHB primary and community medical director Hywel Lloyd said.
"They want fast, agile, responsive primary care services — it’s good that primary care has embraced the health care homes model."
Dr Susie Lawless of Amity Health Centre — the first Dunedin HCH — agrees on the need to put patients first.
"It won’t happen overnight: health care homes is a three-year process to evolve from what we do now to something which is more collaborative and which has quite a different flavour — but at the same time it is business as usual, looking after the healthcare of our patients," she said.
"One of the questions we were asked (when applying) was when we wanted to start, and we said we want to start now because that gives us an opportunity to help shape it, an opportunity to work with the PHO and the DHB to shape what it is actually going to be, and that’s exciting."
The three other practices to become HCHs immediately are the Gore Health Centre, Gore Medical Centre, and Queenstown Medical Centre.
Significant growth in patient and staff numbers in the past five years had prompted Gore Health Centre to pursue HCH status, business manager Rhonda Reid said.
"Many of the changes and initiatives we have identified are included in the HCH programme," she said.
"Changes to procedures will help utilise staff time more efficiently, and better triaging and access to GPs and practice nurses will ensure the patients are being seen by the appropriate person."
Patients would, wherever possible, still see their regular GP, she said.
"We see the HCH programme enhancing this and giving patients more ways to be in contact with their GP."
Alison Wilden, manager of Gore Medical Centre, said becoming an HCH would mean better access to urgent care, and co-ordinated care for those with chronic conditions.
"Providing better long-term conditions programmes should mean that continuity of care can occur even if a patient does need to see a different doctor," she said.
"The development of WellSouth’s long-term conditions management programme will also ensure patients are enabled to manage their conditions with good acute and long-term planning, ensuring they have better health outcomes."
Queenstown Medical Centre GP Richard Macharg hoped HCHs would mean knowledge and resource sharing across like-minded practices, and improved care for all.
"At a practical level, the improvement in access to the practice via both traditional and more innovative routes should be rapidly apparent and help with our stated goal of providing the right care, in the right place, at the right time."
Health Care Homes
Now
Amity Health Centre (Dunedin); Gore Health Centre; Gore Medical Centre; Queenstown Medical Centre.
Later this year
Meridian Medical Centre, Mataora and Broadway Medical Centre (Dunedin); Waihopai Health Services (Invercargill); Junction Health (Cromwell); Wanaka Medical Centre, Aspiring Medical Centre (Wanaka).
Mid-2019
Mornington Health Centre (Dunedin); Alexandra Medical Centre practices (the current Centennial, Cornerstone, and Central Medical practices); North End Health Centre and Junction Doctors (Oamaru); Clutha Health First (Balclutha); Invercargill Medical Centre.











