Two weeks after Gareth Milne had major surgery he lost his wife to breast cancer.
They shared her last days after Milne was moved from Middlemore Hospital where he was recovering from back surgery to his wife Diana's room in Auckland City Hospital.
A photo from the time shows their beds side-by-side. Diana has leaned across to rest her head in her husband's lap. Her eyes are closed. His look down to where his hand rests in her hair.
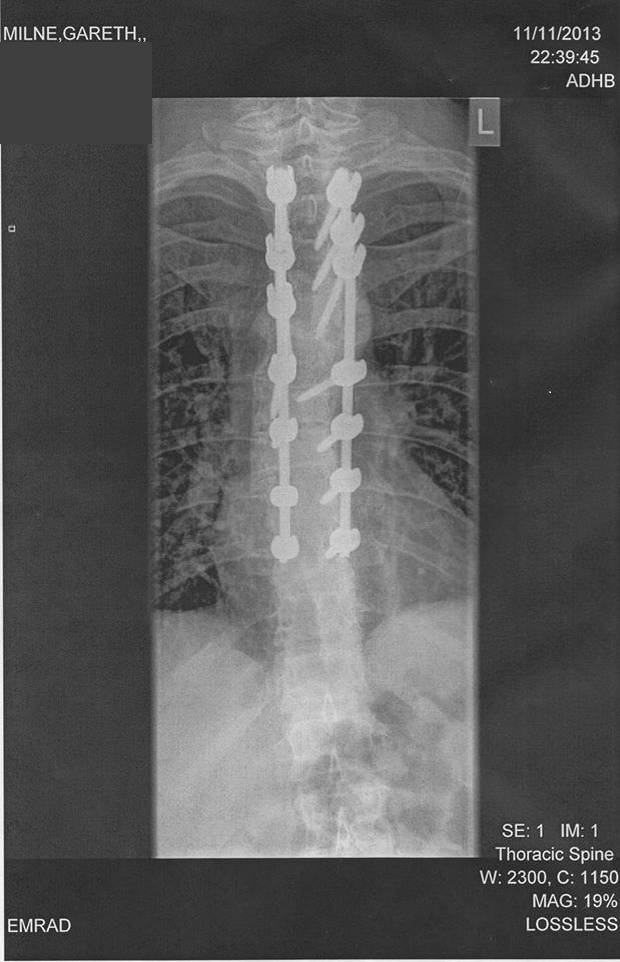
Diana died in November 2013, aged 32. The next month the repair of Milne's back failed when a physiotherapist had him perform the wrong exercises.

"I was feeling as though I had a bit of a light at the end of the tunnel," Milne said of life-changing corrective surgery that's now delayed indefinitely. "But now, I just don't know."
He and Diana married in February 2011. In July she found a lump caused by an aggressive type of breast cancer. Diana was originally from Dunedin and the pair had planned to move there, something Milne stuck with after her death.
"After everything happened I needed a big change."
That's brought happiness - Milne now lives with his partner, Carol, who is also widowed after her late husband died from a brain tumour.
However, Milne's back pain remains. He can manage only about 90 minutes of mobility a day, doesn't sleep much, and has had to give up painkillers after years of use caused stomach problems.
"I still try and do what I can to stay active a little bit, but it's basically pushing the vacuum cleaner around or doing the dishes or something like that," the 43-year-old said.
"I've given up everything I used to enjoy. I had one of my motorbikes sitting in the garage for a while, and I've got rid of that, which was one of my passions.
"I've got no idea of timelines and my memory is really bad now. I think it's all tied in to the stress of it all. I can't think straight anymore like I used to be able to."

Milne was eventually sent to Oamaru Hospital for a scan because of delays in Dunedin. He finally saw a surgeon soon after a complaint was lodged with Southern DHB.
The specialist saw the scan and agreed surgery was needed. It would have a more than 70 per cent chance of success, Milne was told, and on December 5 the DHB sent a letter confirming the operation within four months.
That timeframe hasn't been met - Southern DHB was already struggling with surgery demand, and this worsened after Covid-19 arrived in the country.
Under level 4 restrictions most electives (medical or surgical services that aren't required immediately) were postponed, as hospitals diverted resources and capacity to prepare for any surge in Covid-19 patients.
Some patients needing electives that can't be postponed, including for cancer and trauma injuries, were sent private, but the majority - including hip replacements, cataract removal and endometriosis surgery - were delayed.
Hospitals are gearing up again in level 3, with patients prioritised. The aim is to clear backlogs in an 18-month recovery period, that would take full effect once the country returns to level 2, level 1 and normal status. As in "normal" times, progress and treatment times will differ by DHBs.
Milne has repeatedly tried to find out when his surgery might happen, without success - and his light at the end of the tunnel has dimmed.
"That's what is keeping me going, put simply - being able to live a normal life, it's something I'm still striving for. But, yeah, just have to play it as it comes I suppose.
"I can still walk. So there are people worse off than me, of course. It's just the living in pain thing, it's hard to deal with. I imagine there's a lot of people in the older generations who don't like to cause a fuss and are probably worse off than I am."
Dr Janine Cochrane, Southern DHB's general manager of surgery and radiology, said the Covid-19 response had postponed more than 900 elective surgeries.

"Our thoughts are with the people, like Mr Milne, who have had their elective surgery or other services postponed...and we are very conscious of the need to provide the care they have been waiting for."
The DHB was resuming as much treatment as it could this week, Cochrane said, but there is a significant backlog, and ongoing constraints related to Covid-19 safety protocols. In the next month or two affected patients would be contacted and told an expected timeframe.
"Unfortunately, at this time, we are unable to estimate when patients such as Mr Milne will receive their surgery."
Cancer care under lockdown
More weekend or evening hospital shifts will be needed to deal with a build-up of cancer work caused by the Covid-19 restrictions.
Bowel Cancer NZ medical adviser Professor Frank Frizelle said the big issue for treatment of that disease was about people with symptoms being diagnosed quickly enough.
Covid-19 precautions taken when colonoscopies such as extra personal protective equipment had slowed the process down. That meant patients with obvious symptoms were prioritised over those getting follow-ups for reasons such as family or medical history.
"While you may have done seven or eight patients on a list, now you are doing probably five or six...colonoscopy resources were already pretty tight, and now you slow the volume that can go through down, it's going to put those resources under more strain."
Frizelle said there was a need to "push it a little harder than it's being pushed at the present time" to address the demand, perhaps by working evenings and weekends.
This week the Cancer Society warned up to 400 people could die from cancer if backlogs aren't cleared quickly enough. Under level 4 urgent treatment has continued but there have been fewer scans, tests and surgeries.
A Ministry of Health spokeswoman said the majority of cancer surgeries had continued under level 4, and hospitals were currently reviewing patient lists to prioritise the most needy. Full cancer screening and diagnostic services would resume as soon as possible.
"DHBs, the ministry, the Cancer Control Agency and clinicians are all very aware that people's treatment may have been delayed...the ministry is working with DHBs to develop recovery plans and implement strategies [and] DHBs are advising patients of deferrals and the appropriate steps to take should the patient's condition worsen."












