Health Minister Shane Reti is drawing up the terms of reference for the review with the help of coalition partners, including Act Party leader David Seymour, who campaigned on the issue and successfully passed the country's assisted dying laws through Parliament.
The legislation was rubber stamped after the public voted in favour through a 2020 referendum.
An area Seymour would like to see changed is the eligibility for assisted dying only being available to terminally ill adults with fewer than six months to live.
That compromise was made during the Parliamentary process to appease the Green Party to ensure Seymour got the votes he needed to pass the bill.
Seymour believes the six month timeframe should be scrapped because "it's a shame that some of the people who suffer the worst are still unable to access the law".
"Stipulating a six month timeframe is actually quite cruel," he told RNZ.
Totara Hospice chief executive Tina McCafferty agreed and would "at best like to see that timeframe removed, or extended to twelve months".
"That's because prognosis is both an art and science, and you can't always get that right," she told RNZ.
"It's also a bit at odds with the intention of the Act, which seeks to put the experience and definition of suffering at the hands of the person with terminal illness. The Act says suffering is defined by the patient so we don't see the need for a time requirement to be put on suffering."
The 'gag clause'
Another area where there was consensus for review were the rules that stopped doctors from being able to discuss assisted dying with their patients - with patients needing to raise the medical intervention with their doctor.
Totara Hospice in Auckland is currently the only one in the country that offered the act of assisted dying on its premises.
McCafferty said the "gag clause" on doctors was "at odds with the actual responsibilities of healthcare professionals, where there's an obligation to inform patients of all choices they can have in their care".
She wanted that clause removed because "there's a bias in that it leaves it up to articulate patients to raise their needs in that way".
"Not everyone is articulate when it comes to health literacy, and I want to see that potential bias or inequity mitigated."
Hospice NZ chief executive Wayne Naylor said the so-called gag clause was challenging "because you don't want to put that idea into someone's head if they haven't thought of it, but we're also thinking about a person's right to have all the options laid out in front of them before they make a decision".
He wanted some clarity on that clause to come out of the review, along with provisions for bereavement and grief support for the family of those who used assisted dying.
"We still don't see assisted dying as part of palliative care or what hospices do, but certainly they shouldn't be in any way blocking or preventing a person pursuing that if that's what their wish is."
Naylor said hospices' approach to assisted dying had evolved a lot, but warned against changes being made to the laws based on a small number of complaints.
"In the beginning it was very challenging and unclear to some extent how some hospices should respond. Certainly over the last three years there's been a change."
He said the majority of hospices now allowed assessment for eligibility of assisted dying to take place on site and support services were extended to families who had a loved one use assisted dying.
"The only thing that's still the same is hospices generally don't offer the actual act of assisted dying on their premises, with the exception of Totara Hospice."
Law change at mercy of Parliament's biscuit tin
The review of assisted dying laws is required to happen this year, but it could be years before any changes are made, if at all.
Seymour told RNZ the review will "not in itself change the law" because the outcome is a report to Parliament that will likely have some recommendations, but there was no requirement for the government to pick up the changes or Parliament to debate it.
It's more likely an MP - possibly one from Act - will take the recommendations and put them into a member's bill, which will need to be pulled from the ballot to be considered.
Seymour said the coalition government had to "speak with one voice" and that was difficult with a conscience vote issue like assisted dying.
"I know there are people in the Cabinet who would say it would actually conflict with their conscience to have to support this legislation."
As of 31 January, there had been 1775 applications for assisted dying - 980 were approved and 681 of those followed through on it.
On average, from the time an application is made to written approval being received, the Assisted Dying Service advised it was a four to six week process.
While there was agreement on some of the ways the laws could be extended, there were others who thought the changes should go much further.
Napier's Glenn Marshall wants to see assisted dying made available to those who make their wishes clear in an advanced directive before their illness means they lose the option altogether.
Glenn and Fran Marshall's profoundly intellectually disabled son Eamon died last year after five days in care receiving palliative sedation therapy.

Glenn Marshall described the way his son died as "barbaric" with many interventions, including cessation of food and fluids, taking place.
He objected to palliative sedation therapy being used so freely, while there were so many rules and restrictions to assisted dying, when he believed the two interventions were the same.
That opinion was not shared by Naylor and McCafferty, who both described palliative sedation therapy as a mechanism for relieving suffering and distress and said the underlying illness a patient was suffering was the cause of death.
Naylor did acknowledge "a person may die a little sooner than they otherwise would have", but said that was a secondary consequence whereas the primary aim of assisted dying is to end a person's live with the administration of a life-ending medication.
McCafferty added the cessation of food and fluids happened because "a person's body is at the point of death that it can no longer cope with processing fluid or foods".
"It's often mistaken that they're being actively withdrawn, and that's not actually the case, it's that the body can no longer process them."
McCafferty did say the country did need to have a better look at palliative sedation, which included the withdrawal of life-sustaining treatments.
"For many years of practice there have been ways that have not been explicitly identified as hastening death, but which certainly don't sustain life."
The 'dementia tsunami'
Marshall's motivation for fighting for better assisted dying laws was to ensure there was more options for people to choose when they had a sound mind to make the decisions.
"People should be able to do an advanced directive to say, 'if this happens to me, be it demential or a serious car accident or whatever, if I find myself in x, y or z situation, this is what I'd want to happen to me'."
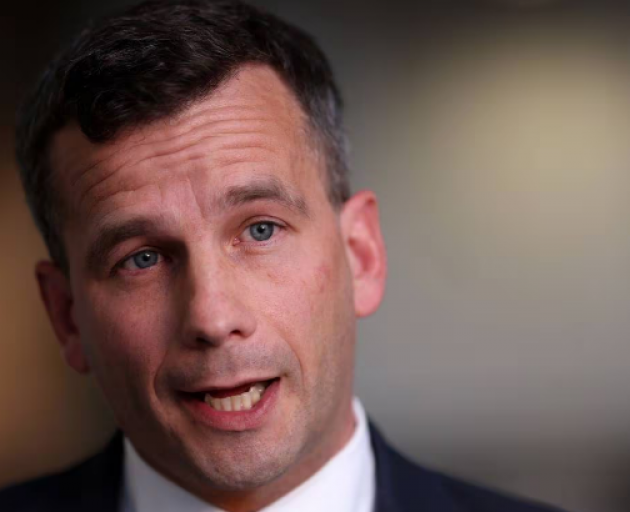
Seymour maintained he always campaigned on the basis assisted dying had to be a person's choice and that person had to be capable of making that choice.
"For me children have always been out, people who have lost the capacity to decide for themselves are out.
"I'm still open to being convinced, but there's a very big moral difference between someone making the decision for themselves and for someone else," he told RNZ.
Assisted dying had always been utilised by "the more educated, the more assertive, and more wealthy people", according to Seymour.
"You actually have to be pretty assertive to get to access it and navigate the system in the first place. That's one of the reasons why assisted dying affecting vulnerable people was never a true argument no matter how often it was trotted out.
"I think we're now in a space where we can have a discussion about things like, can a doctor in the right circumstances raise the subject of assisted dying - the current laws say it cannot - but it's also true that in the natural cause of events a doctor has an obligation to raise all the possibilities that might be appropriate for you," Seymour said.
While it was the assisted dying laws up for debate and review, Naylor told RNZ it was palliative care that continued to need a real focus from the government.
"Assisted dying I think is working okay, there's a few tweaks to fix it, the whole palliative care and hospice sector is desperately in need of more funding and workforce."
About 34,000 people died from a predictable death last year and all of them would have benefited from palliative care, he said.
"A large number of them aren't getting the end of life care they should get. Assisted dying is fully funded, you can get it wherever you want, that's not the same for palliative and hospital care.
"There are large parts of the country that don't have good access. We need the government to focus on that part," Naylor said.
The Health Minister told RNZ work on the review was in the early stages and ministers were considering what the terms of reference should be.
Reti, who voted against the End of Life Choice Act, says he took all aspects of his portfolio "extremely seriously" and this review was no different in terms of its importance.
"The Prime Minister passed ministerial responsibility for this to me... at all times, and as the public would rightfully expect, I will be working closely and appropriately with the Ministry on it."
Reti disagreed with Marshall that palliative sedation therapy was a form of physician-assisted death.
"As a physician, I understand that palliative sedation results in a death that is without suffering, is comfortable and calm and ensures the person is unaware. It would generally be considered a dignified death."
The Assisted Dying Service was set up in November 2021 and as of last December the cost to run it has been $4.77 million. Its operational costs were spread between the Ministry of Health and Te Whatu Ora and were not tracked separately so that figure was unavailable.
"Health NZ currently provides or funds services for those with palliative or end-of-life care needs across a range of care settings including hospitals, specialist services, primary care, aged residential care, home and community support and hospices," a Te Whatu Ora spokesperson said.
Most of those services were bulk funded so it was not easy to say what the exact costs of palliative care were, but of the 28 hospices funded by Health NZ - which deliver only palliative care and no other services - $113.6m in funding was received for the 2023/24 financial year.