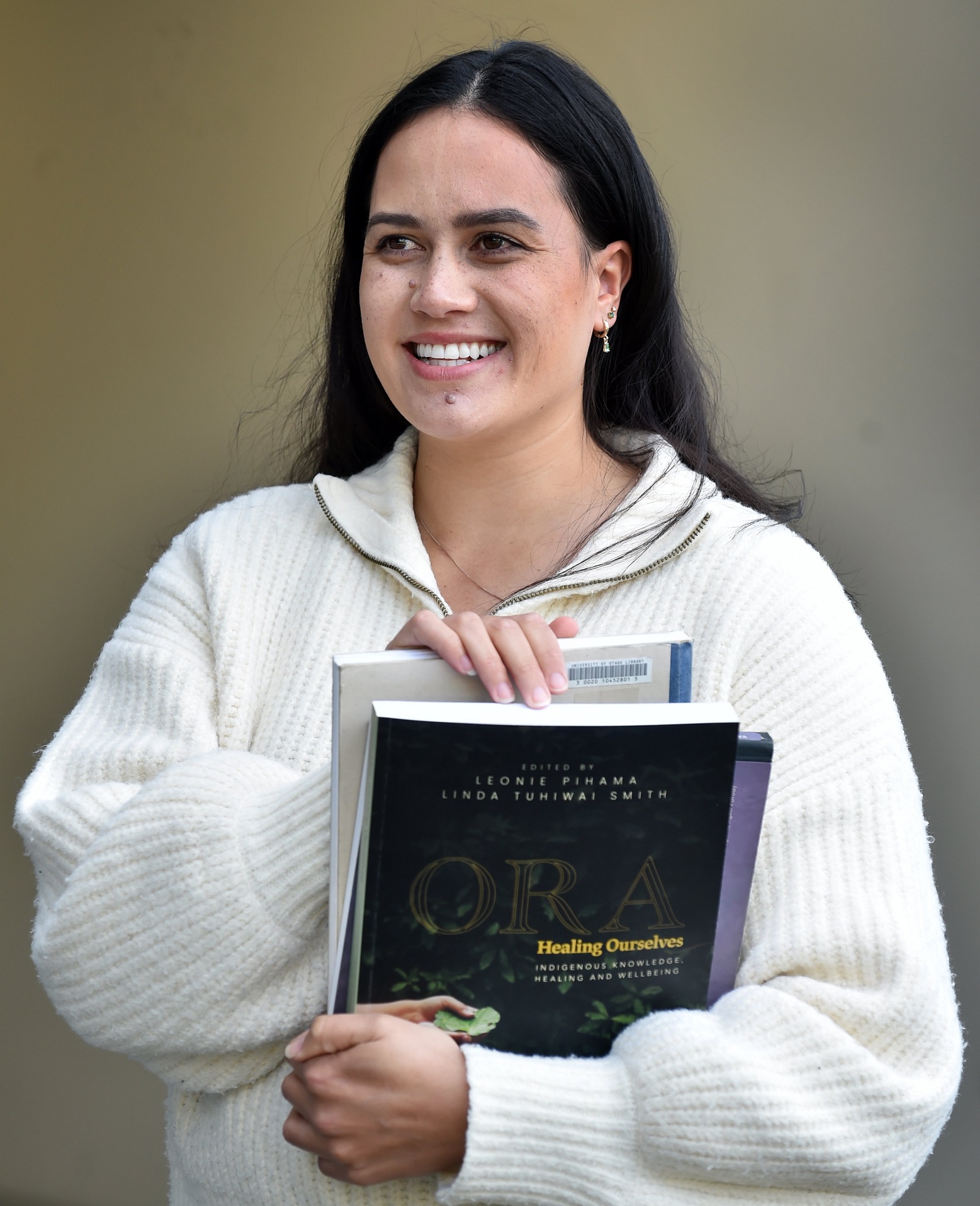
University of Otago psychology PhD candidate Felicia Lawrie (Ngāti Kahungunu, Ngā Puhi) is the lead author of the study.
It explored Māori women’s experiences with childbirth in New Zealand’s healthcare system.
Mrs Lawrie said it was important to find ways to make births more culturally affirming and positive for Māori women.
"We are in a system that has, unfortunately, failed our wāhine Māori.
"We are at higher risk of postnatal depression, anxiety, PTSD ... [and] 3.4 times more likely to die by suicide than non-Māori mothers — we need change."
She was inspired by her "own lived experience".
"I gave birth to my son by emergency Caesarean section just over five years ago.
"I wanted my research to provide a space for others to share their stories and how we can better meet the needs of Māori mums, specifically within the space of Caesarean sections."
She had her son in Australia, seven weeks before moving to New Zealand.
Although she was dealing with a different healthcare system, she found there were many similarities between her story and those who participated in her study.
After a very long labour, it was decided a Caesarean labour was the "best way forward".
"I would have liked to have been told more about it.

Most women in her study had similar experiences and wished they were "presented with all the options".
"They still may have chosen to have a Caesarean delivery, which is great, but at least they would have had a choice."
Mrs Lawrie started research in 2022 with help from Dr Amanda Clifford.
Her research showed being able to have a choice during childbirth played a vital part in whether or not the experience was positive.
For her second child, she had a vaginal birth at the Queen Mary Maternity Hospital in Dunedin.
It was "one of the best experiences of [her] life" and she felt lucky to have an "extremely caring" midwife who was supportive of the birth she wanted to have.
The decision to abolish Te Aka Whai Ora was "really disappointing" as it had many great initiatives to support Māori women.
"Te Aka Whai Ora ... was an opportunity for change in a system that’s failing Māori."
It provided services to help Māori women find midwives, transport to prenatal appointments, blood tests, classes on traditional practices and how they can be incorporated in labour and delivery, as well as overall help navigating a system not made for them.
Mrs Lawrie encouraged people to take the time to listen to peoples experiences, hear them and believe them.
"The birthing experience of the mother and the baby impacts the rest of the child’s life, the mother’s life and the whole whānau and then generations to come as well."












